Transform payer contracts
into revenue opportunities
with Aroris360™
The only healthcare contract management software built specifically
to maximize your reimbursement rates. Aroris360 digitizes your contracts,
monitors every claim payment, and ensures you collect every dollar you’ve negotiated.
Results you can count on
Average reimbursement rate
increase for clients
Highest rate increase on
a payer fee schedule
Number of practices served
throughout the U.S.
The challenge: Navigating the bureaucracy of healthcare reimbursement
You got into medicine to heal people, not to spend your days cutting through the red tape of healthcare reimbursement. And yet today, managing payer contracts is the biggest financial challenge practices face.




Hidden Revenue Loss
Payers routinely underpay against contracted rates, and most practices never catch it. Without systematic monitoring, you’re losing revenue on every claim.
Manual Monitoring Failures
Healthcare providers often lack dedicated staff with specialized expertise in contract management and negotiation. 42% of physicians spend more than 10 hours weekly on payer negotiations and related activities, taking valuable time away from patient care.
Data and Information Gaps
Providers have limited visibility into market-rate benchmarks and competitive reimbursement data. Without these insights, it’s impossible to know if rates are fair. Research reveals up to 300% variation in insurance reimbursement rates for identical services across different payers.
Administrative Overwhelm
From tracking renewal dates to monitoring compliance with contract terms, the administrative burden is substantial. Most practices work with multiple payers, each with different requirements and procedures, yet the day-to-day demands of patient care leave little time for contract analysis.
Power Imbalance
Payers have teams of negotiators, attorneys, and data analysts, while providers often have limited negotiation resources. This creates a significant power disparity between large insurance companies and individual medical groups.
The Solution:
Aroris360 Contract Management Platform
Aroris360 is the only contract management software designed specifically for healthcare reimbursement optimization.
Built by healthcare administrators, contract attorneys, and data engineers with 50+ years of combined industry experience, it digitizes every contract, analyzes payer and code mix, and benchmarks rates against the market to uncover hidden revenue.
The result? Less manual work, more visibility, and the confidence that every claim is paid as promised.
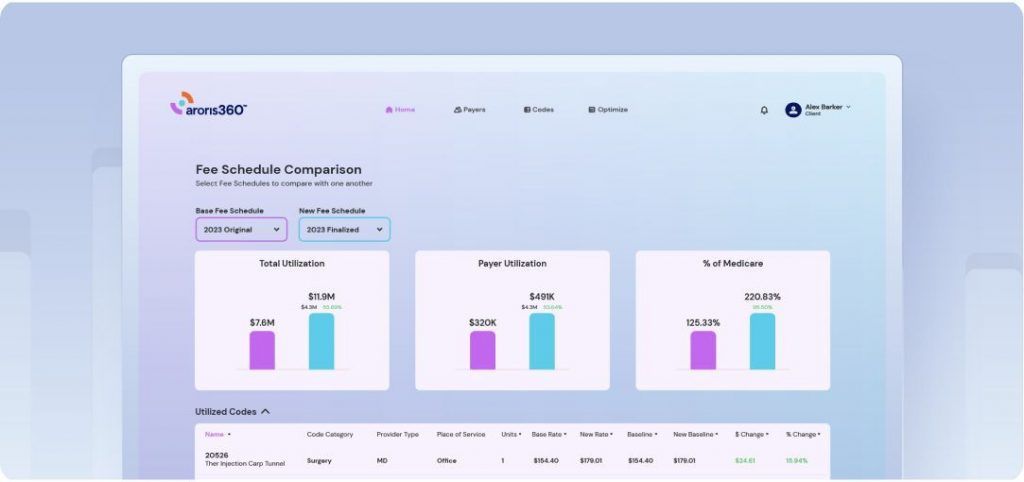
How Aroris360 works
Aroris360 turns complex payer contracts into clear revenue opportunities through our proven process:
DIGITIZE
Build a strong foundation by centralizing and organizing all payer data.
Digitized Payer Contracts
Transform paper contracts into a searchable digital library, allowing instant access to terms, side-by-side comparisons, and automated compliance alerts—streamlining renewals and strengthening negotiating leverage.
Digitized Fee Schedule Library
Provide a centralized, digital repository of all fee schedules—enabling healthcare organizations to easily store, update, compare, and analyze fee structures across different payers, service lines, and time periods.
Claims Data Integration Direct
Connection to clearinghouse 835/837 files for real-time payment data processing, comprehensive claims history, and automated payment verification.
ANALYZE
Understand exactly where you stand and where revenue opportunities exist.
Payer Mix Breakdown
Analyze the distribution of charges across multiple payer types (e.g., Medicare, Medicare Advantage, Medicaid, Commercial, Self-Pay) to understand each type’s impact on revenue and help healthcare organizations make data-driven decisions.
Code Mix Review
Visualize practice utilization by your top codes to understand revenue patterns and optimization opportunities.
Detailed Code Insights
Provide a comprehensive view of all billing codes—including their reimbursement rates, volumes, and utilization patterns—so organizations can pinpoint revenue opportunities, optimize billing, and negotiate more effectively across different payers.
Code Level Reimbursement
Surface the exact reimbursement rate for every code—broken out by payer, place of service, and geography—so your team can spot underpaid services, recoup missed revenue, and negotiate rate increases with data in hand.
STRATEGIZE
Leverage your market position to negotiate better terms and maximize revenue.
Market Transparency & Benchmarking
Equip healthcare organizations with data-driven insights to compare their fee schedules, reimbursement rates, and operational metrics against broader market averages. This enables practices to gauge competitiveness, identify growth opportunities, and refine strategies for optimal financial performance.
Competitor Transparency & Benchmarking
Provide healthcare organizations with a detailed understanding of how they stack up against direct competitors in terms of pricing, reimbursement rates, and operational practices. By identifying strengths and weaknesses relative to peers, practices can make strategic decisions to enhance competitiveness and boost revenue.
Client Payer Benchmarking
Provide a centralized, data-driven approach to evaluating payer performance—enabling healthcare organizations to compare contract rates and overall reimbursement effectiveness across different payers. This empowers practices to pinpoint areas for improvement, optimize negotiations, and enhance financial outcomes.
Medicare Benchmarking
Compare your organization’s reimbursement rates and billing practices to local and national Medicare benchmarks—offering a clear gauge of whether payments align with accepted industry standards.
Expert Negotiation Support
Access to healthcare contract negotiation specialists including former payer executives, healthcare administrators, and contract attorneys who bring insider knowledge to every engagement.
REALIZE
Ensure every negotiation dollar makes it to your bank account.
Live Claims Monitoring
Track every claim as it processes through payer systems with automated payment verification against contracted rates. Receive instant alerts when payments fall below contracted rates or when claims are processed incorrectly, enabling immediate action to protect your revenue and recover underpayments that would otherwise go undetected.
Payment Integrity
Continuously track and review your claims to ensure accuracy in reimbursements, quickly identify underpayments or errors, and protect your revenue stream through systematic monitoring and validation.
OPTIMIZE
Turn insights into sustained revenue increases.
Renewal Management
Never miss a contract renewal opportunity again. Automated alerts ensure you’re always prepared to negotiate better terms with comprehensive data and strategic timing.
Historical & Quarterly Medicare
Keep your organization aligned with the latest Medicare fee schedule changes—both nationally and locally—by automatically pulling new rates from CMS on a quarterly basis, while preserving historical data for trend analysis.
How we’re different
Traditional Contract Management
- Underpayments go undetected
- Static document storage
- Generalized for all industries
- Focus on compliance only
- Limited negotiation support
- No market benchmarking
- Reactive to problems
Aroris360 Approach
- 24/7 Live claims monitoring
- Dynamic analysis and data visualization
- Healthcare-specific intelligence
- Focus on revenue optimization
- Expert negotiation services available
- Robust competitive data
- Proactive opportunity identification
Your all-in-one platform to digitize
contracts, negotiate higher reimbursements
and drive higher revenue.
Flexible Partnerships
You’ll never hire one person who can digitize every payer contract, analyze your rates, and negotiate against national payers. We offer several straightforward options to meet your organization’s needs.
FAQ
Have questions? Aroris has the answers.
Don't see your question? Ask an Aroris representative.